Stroke
About Stroke
Stroke occurs when a blood vessel is compromised and unable to deliver oxygen and nutrients to the brain, resulting in the death of parts of the brain and an accompanying loss of functions. This may result from an occlusion of arteries, known as an ischaemic stroke, or from a rupture of cerebral arteries, causing a haemorrhagic stroke 1Campbell, B. C. V. & Khatri, P. Stroke. Lancet, 396, 129-142 (2020).
Stroke is a leading cause of death and disability worldwide, with 1 in 4 people afflicted by stroke in their lifetime. The incidence rate of stroke is estimated to be nearly 14 million per year, of which 70% are ischaemic, and the remaining 30% haemorrhagic 2Phipps, M. S. & Cronin, C. A. Management of acute ischemic stroke. BMJ, 368: 16983 (2020).
In China, stroke is the top cause of death and disability, presenting high incidence, relapse, disability, and mortality rates. Acute ischemic stroke (“AIS”) accounts for around 70% of the stroke incidents in China and is estimated to increase from 3.6 million in 2020 to 5.8 million in 2030 3,Campbell, B. C. V. & Khatri, P. Stroke. Lancet, 396, 129-142 (2020) 4Wang, W. et al. Prevalence, Incidence, and Mortality of Stroke in China: Results from a Nationwide Population-Based Survey of 480 687 Adults. Circulation, 135, 759-771 (2017), With the growing and aging population, the number of new cases of AIS continues to increase.
Ischaemic stroke
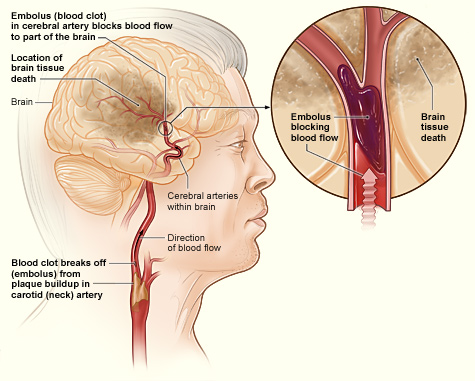
Most ischaemic strokes directly result from thromboembolism, where a blood clot becomes stuck in a blood vessel, obstructing the flow of blood. This may arise from large artery atherosclerosis or heart diseases 1Campbell, B. C. V. & Khatri, P. Stroke. Lancet, 396, 129-142 (2020). In atherosclerosis, fats, cholesterol, and other substances forms a plaque along the arterial walls. Rupture of the plaque induces the formation blood clots that can travel downstream to occlude large vessels relevant to stroke. An irregular heartbeat, medically known as atrial fibrillation, allows blood to stagnate and clot. These clots eventually flow downstream and cause occlusion of the cerebral arteries. Less commonly, ischaemic strokes find their origins in small vessel disease, arterial dissection, and arterial inflammation 5 Campbell, B. C. V. et al. Ischaemic stroke. Nat Rev Dis Primers, 5, 70 (2019)..
Haemorrhagic stroke
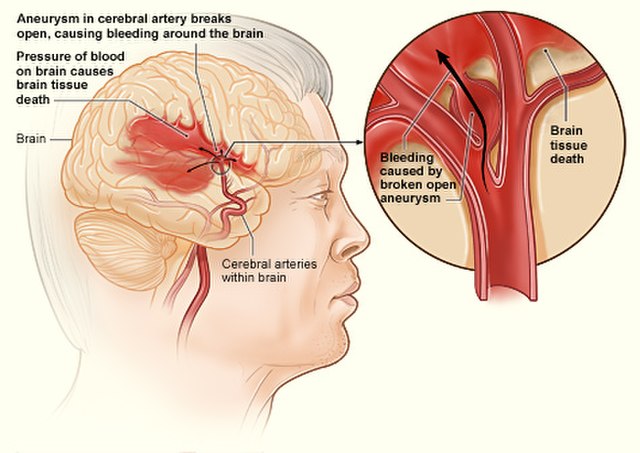
Haemorrhagic strokes can be intracerebral or subarachnoid, where the former refers to bleeding within the brain tissue, and the latter refers to bleeding that is outside of the brain tissue but still within the skull 6 Centers for Disease Control and Prevention (2021). Types of Stroke. Retrieved from: https://www.cdc.gov/stroke/types_of_stroke.htm.. Major causes include aneurysms associated with high blood pressure, and amyloid angiopathy, where there is disease of the blood vessels arising from the accumulation of amyloid proteins along its walls 1 Phipps, M. S. & Cronin, C. A. Management of acute ischemic stroke. BMJ, 368: 16983 (2020).. An intracranial aneurysm is a weak or thin spot on an artery in the brain that balloons and fills with blood. The bulging aneurysm can put pressure on the nerves or brain tissues, manifesting as visual impairment, difficulties in speaking or concentrating, and loss of balance among others. The most serious sequela of intracranial aneurysms is aneurysm rupture and subsequent subarachnoid hemorrhage (SAH), with a mortality rate of 3 in 5, and a 1 in 2 probability of causing a neurological disease in survivors 7 NHS (2018). Brain aneurysm. Retrieved from: https://www.nhs.uk/conditions/brain-aneurysm/.
Risk Factors
Non-modifiable risk factors for ischaemic stroke include age, sex and genetic factors.
Research indicates that around 90% of strokes are attributable to modifiable risk factors such as:
- High blood pressure
- Smoking
- Diabetes
- Diet
- Physical inactivity,
- Obesity
- High blood
- cholesterol
- Carotid artery disease
- Peripheral artery disease
- Atrial fibrillation
- And Other heart diseases.
Treatment Paradigm For Stroke
Management of stroke in an organised and geographically defined stroke unit, delivering evidence-based clinical protocols, has been shown to yield the best outcomes. Benefits from such stroke units staffed by a dedicated health team comprising medical, nursing, and allied health professionals, may stem from the prevention of complications, and early secondary prevention and rehabilitation. 1, Campbell, B. C. V. & Khatri, P. Stroke. Lancet, 396, 129-142 (2020) 6Centers for Disease Control and Prevention (2021). Types of Stroke. Retrieved from: https://www.cdc.gov/stroke/types_of_stroke.htm
In ischaemic stroke, the obstruction of blood flow leads to a cessation of neuronal function and tissue damage, which is exacerbated with an increasing amount of time before treatment. Treatment involves re-establishing blood flow to the affected brain tissue, and if timely administered, can restore function to the ischaemic penumbra to substantially reduce disability after the disease. Typical treatment for acute ischaemic stroke is currently defined by intravenous thrombolysis closely followed by mechanical thrombectomy 1 Campbell, B. C. V. & Khatri, P. Stroke. Lancet, 396, 129-142 (2020)
Intravenous injection of thrombolytic drugs like recombinant human tissue plasminogen activator (rt-PA) seeks to dissolve the clot for reperfusion. Two main drugs, namely alteplase and tenecteplase, lead the charge in this mode of treatment. rt-PA treatment is limited by its treatment window – a meta-analysis of nine randomised trials found that rt-PA gave clear clinical benefits when administered within 3.0 – 4.5 hours of stroke onset 9Emberson, J. et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet, 384, 1929-1935 (2014). Yet less than 1 in 4 stroke patients in China obtain medical attention within this window of effectiveness, such that rt-PA utilisation is only 1.6% 10Wang, Y. et al. Using recombinant tissue plasminogen activator to treat acute ischemic stroke in China: analysis of the results from the Chinese National Stroke Registry (CNSR). Stroke, 42, 1658-1664 (2011).
. rt-PA treatment also bears the inherent risk of haemorrhage that worsens cerebral injury, such that patients with increased risk or intracerebral or systemic bleeding may have to be excluded 6Centers for Disease Control and Prevention (2021). Types of Stroke. Retrieved from: https://www.cdc.gov/stroke/types_of_stroke.htm. Notwithstanding, intravenous thrombolysis is the most accessible reperfusion therapy for stroke since mechanical thrombectomy is restricted to major stroke centres whilst unavailable in many parts of the world.

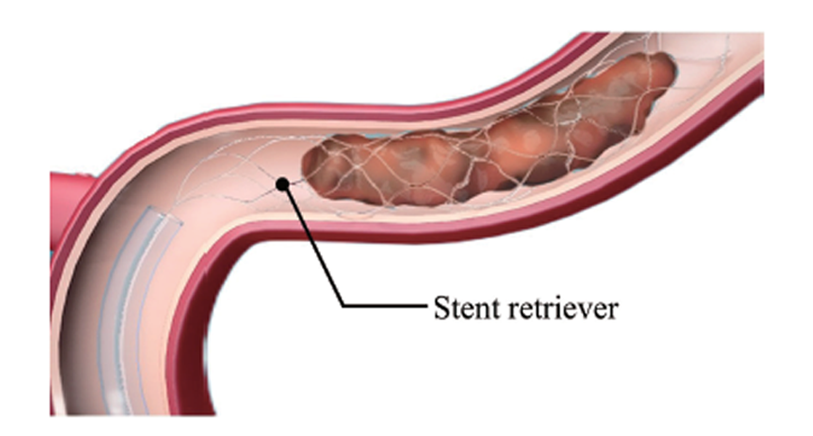
Mechanical thrombectomy is the imaging-guided removal of a blood clot using stent retrievers and/ or aspiration catheters. Both devices are navigated to the site of the occlusion and seek to remove the clot, either by capturing it in its stent struts, or in the case of the aspiration catheter to retrieve the clot with constant negative pressure.
Mechanical thrombectomy comprises aspiration (ADAPT), stent retrieval (SR), and the combination of both. In aspiration, an aspiration catheter is operated to directly aspirate a blood clot and restore a blocked vessel, being one of the most innovative and fastest growing therapies in recent years with promising efficacy and safety. The following diagrams illustrate in further detail the thrombus aspiration process during the main part of a procedure.
ADAPT (a direct aspiration first pass technique) utilizes aspiration as the first-line strategy to restoring blood flow to a blocked vessel. ADAPT has been gaining popularity primarily attributable to inherent versatility, speed, and lower costs relative to stent retriever methods, while clinically shown to be as safe and effective in clearing cerebral vessel occlusions. ADAPT also facilitates a higher rate of complete clot ingestion with minimal fragmentation, leading to a higher rate of first-pass complete recanalization and fewer distal emboli 12, Turk, A. S. et al. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet, 393, 998-1008 (2019) 13Goyal, M. et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet, 387, 1723-1731 (2016).
Stent retriever (SR), a major type of ischaemic stroke treatment device, is a self-expanding stent that is deployed to entrap a blood clot within the stent struts before both are withdrawn back into the catheter.